Intrauterine devices (IUDs) have surged in popularity recently as a convenient, long-term birth control method.
Modern IUDs are also highly effective, with less than a 1% chance of unintended pregnancy each year. Yet, despite significant improvements, there are still some myths around IUD safety and side effects. And when it comes to your reproductive well-being, you wouldn’t want these misconceptions to affect your decision.
If you’re considering an intrauterine device (IUD) as a contraceptive option, separating fact from fiction is crucial. The abundance of information out there can be overwhelming, especially when some myths might dissuade you from exploring this effective birth control method.
In this article, we will debunk eight common IUD myths to provide you with accurate information and help you make informed decisions about your reproductive health.
Table of Contents
Myth #1: There Is Only One Type of IUD Available
Wrong!
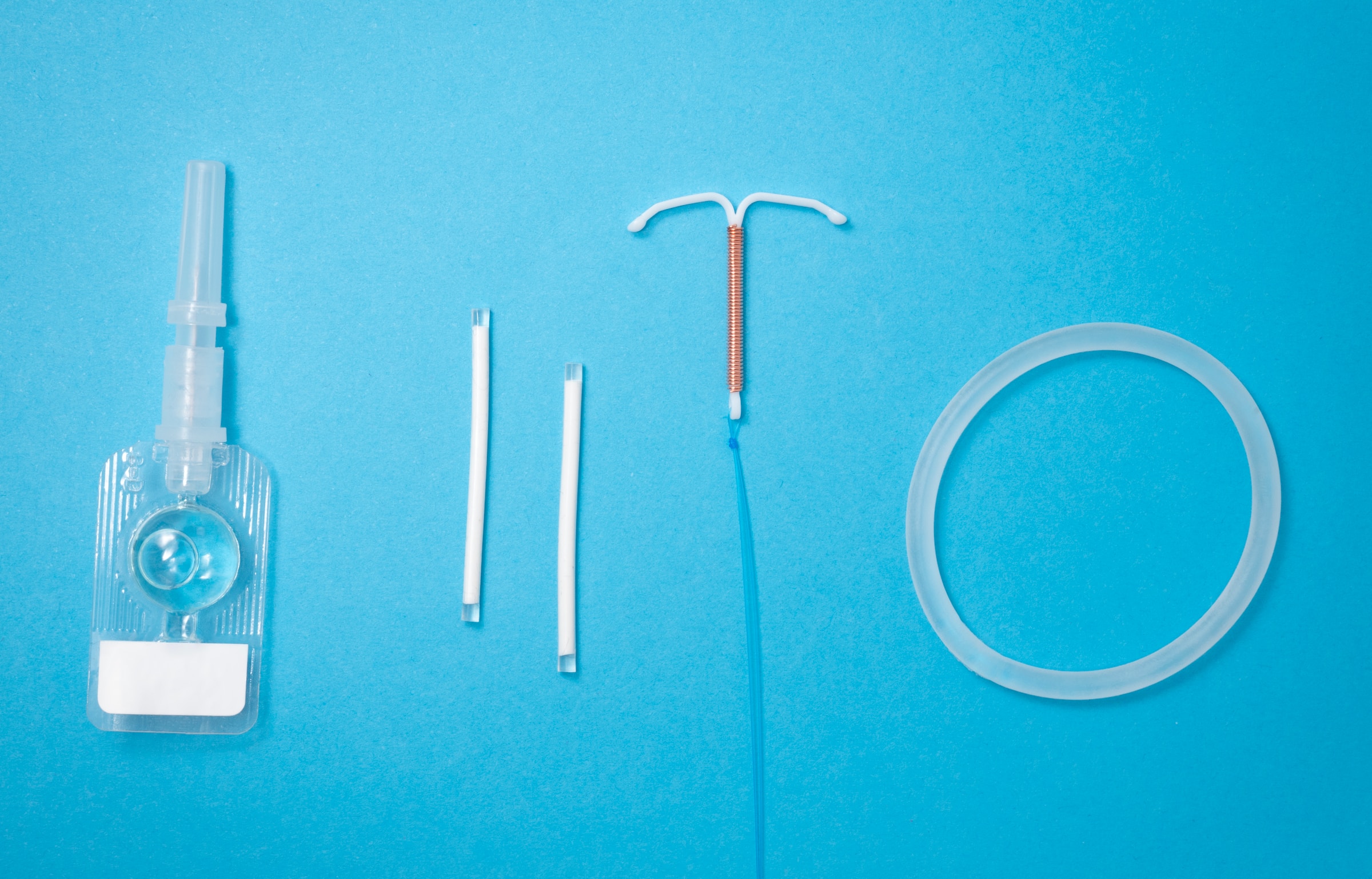
Just like shoes come in different styles, IUDs do, too. Modern IUDs come in two main categories based on shape: T-shaped hormonal IUDs like Mirena, Skyla, Liletta, or Kyleena, and copper non-hormonal IUDs like Paragard.
Hormonal IUDs release tiny amounts of progestin, which trims your uterine lining and thickens the cervical mucus. This makes it challenging for sperm to fertilize the egg. On the other hand, copper IUDs work by creating a hostile environment for the sperm, thus avoiding fertilization.
Within each IUD category, there are also multiple options in varying sizes and with differences in the recommended duration of effect. Understanding these options is crucial when considering an IUD, as it allows women to choose the type that aligns best with their bodies and lifestyles.
Myth #2: IUDs Are Expensive and Inaccessible
While IUDs initially cost more than some other birth control methods, their long-lasting effectiveness makes them cost-effective in the long run.
However, thanks to the Affordable Care Act, all FDA-approved contraceptive methods like IUDs are now covered at no out-of-pocket cost by private plans. Medicaid expansions have further increased accessibility and affordability for lower-income women.
While obstacles still exist for some demographics, most American women can now receive their preferred IUD at no personal cost if desired. So concerns about expense or coverage limitations should no longer deter those interested in long-acting, reversible IUD contraception.
Myth #3: IUDs Cause Severe Side Effects
You may come across anecdotes of women who experienced severe muscle spasms, heavy bleeding, or intolerable pain after IUD insertion. This fuels the fear that side effects are a given.
However, over 80% of women report being very satisfied with their IUD overall. In clinical studies, average satisfaction scores exceeded 3 out of 5 across both hormonal and non-hormonal options.
While some discomfort is normal after any new birth control method, including IUDs, it doesn’t always translate to “severe.” The most common side effects are mild and temporary, like muscle spasms, irregular menstrual bleeding, spotting, or breast tenderness. These usually subside within a few weeks or months as your body adapts to the IUD.
Serious side effects like expulsion or perforation are extremely rare. The overall IUD expulsion rate ranges from 2% to 29.8%, whereas 1 out of 1,000 IUD insertions can experience uterine perforation. However, this risk is slightly higher for women who have just given birth and are still lactating.
Regular checkups with your doctor can help catch any potential issues early and manage any lasting ones as well.
Myth #4: IUDs Are Painful to Insert or Remove
Pain is subjective. This is why you’ll hear some women say, ‘It’s as painful as childbirth,’ whereas others say, ‘I’ve dealt with worse.’
IUD insertions are minimally invasive, and doctors even use local anesthesia to reduce the discomfort. Once the IUD is inserted, you’ll feel discomfort as your body adapts to it. At worst, the pain feels similar to a heavy period cramp, but it typically subsides within a few days.
Removal is quicker and less painful than insertion. While rare, some women with non-hormonal IUDs have reported severe pain and discomfort during these procedures. There have also been thousands of Paragard lawsuit allegations claiming that the copper IUD breaks upon removal, causing severe injury.
According to Torhoerman Law, over 2,200 lawsuits have been registered against Teva Pharmaceutical and Cooper Surgical, the manufacturers and suppliers of the IUD devices. This information shouldn’t stop you from exploring your IUD options; rather, it should encourage you to stay updated with the latest IUD developments and legal proceedings.
Myth #5: IUDs Can Migrate and Get Lost in the Body
IUDs are positioned in your uterus and secured with strings that your doctor can easily check during your regular checkups.
While rare, the possibility of an IUD migrating exists, but it’s not synonymous with being ‘lost’ in the body. In most cases of displacement, women do notice changes like pain or bleeding that prompt them to get checked. So fears of an IUD dislodging without your knowledge are somewhat inflated.
To sum it up, IUDs are a safe, effective, and accessible birth control option for many women.
Don’t let misinformation hold you back from exploring this option. By debunking these myths and arming yourself with accurate information, you can make informed choices about your reproductive health and find the birth control method that’s right for you.
Remember, your body is your choice! And always consult a healthcare professional to discuss your specific needs and




Wow superb blog layout How long have you been blogging for you make blogging look easy The overall look of your site is magnificent as well as the content
order lipitor 10mg generic lipitor 80mg without prescription lipitor 20mg generic
order cipro 1000mg – augmentin 1000mg tablet amoxiclav pills
purchase ciprofloxacin pills – bactrim pills augmentin without prescription
oral ciplox 500 mg – order trimox sale
oral erythromycin 500mg
buy generic metronidazole for sale – buy clindamycin pill order zithromax 250mg without prescription
ivermectin 12mg without prescription – sumycin canada buy tetracycline 250mg pill
order valacyclovir pills – buy acyclovir 400mg without prescription buy acyclovir 400mg online
acillin brand buy doxycycline for sale amoxicillin over the counter
oral metronidazole – metronidazole 200mg cost zithromax us
furosemide 100mg tablet – purchase lasix pills captopril buy online
metformin 1000mg oral – metformin 1000mg generic buy lincomycin online
retrovir 300mg generic – irbesartan 150mg ca order zyloprim pills
buy clozapine 50mg – buy clozapine 100mg generic buy pepcid 20mg for sale
order quetiapine 50mg generic – effexor 75mg tablet buy eskalith pills
cost clomipramine – order paxil 10mg buy doxepin pills for sale
atarax over the counter – buy generic prozac online buy amitriptyline 10mg for sale
oral augmentin 1000mg – ampicillin pills buy baycip tablets
buy amoxil online – order generic duricef 250mg buy cipro 1000mg online cheap
where can i buy zithromax – metronidazole canada ciprofloxacin 500mg over the counter
cleocin 150mg drug – terramycin generic where to buy chloromycetin without a prescription
You seem to have an uncanny understanding of this topic! Your knowledge is so extensive, it’s as if you penned a comprehensive book on it. While adding a few images to enhance the message might be a small improvement, your blog is already outstanding. It’s been a truly enjoyable read, and I’ll definitely be returning for more. By the way I am a Senior Researcher @ Clickmen™ ~ SEO Experts & Backlink Building Web Design Agency in USA & Canada.
ivermectin side effects – cheap levaquin order cefaclor 500mg
strongest over the counter antihistamine – ventolin 4mg brand order theo-24 Cr 400mg online cheap
methylprednisolone 16mg over the counter – how to get fml-forte without a prescription buy generic azelastine
cheap clarinex – order triamcinolone 4mg for sale order ventolin generic
micronase 2.5mg us – order micronase 2.5mg dapagliflozin buy online
glycomet over the counter – buy losartan no prescription precose pills
buy prandin without prescription – empagliflozin order order jardiance 10mg pills
semaglutide 14 mg drug – desmopressin ca how to buy desmopressin
order lamisil pills – order fluconazole 200mg buy griseofulvin generic
order nizoral – purchase lotrisone online cheap buy itraconazole online
best india pharmacy https://indiaph24.store/# india pharmacy
best india pharmacy
famciclovir 500mg over the counter – valcivir order buy valaciclovir cheap
digoxin 250 mg canada – dipyridamole us buy lasix diuretic
https://ciprofloxacin.tech/# п»їcipro generic